The Microbiota-Gut-Brain Axis: Definitely More than a Gut Feeling
By Pablo Cataldo, PhD
Have you ever struggled with an experiment until you finally had "a gut feeling" about a possible new approach or protocol modification? Many of us usually "go with our gut" or "follow our gut instinct" to the lab bench and hope for the best. Also, how many of us have felt "butterflies or a knot in our stomach" just minutes before a poster presentation or oral communication? All these sensations are typical examples of how a response in the brain is translated into the gut.
The Gut-Brain Axis: A Scientific Reality
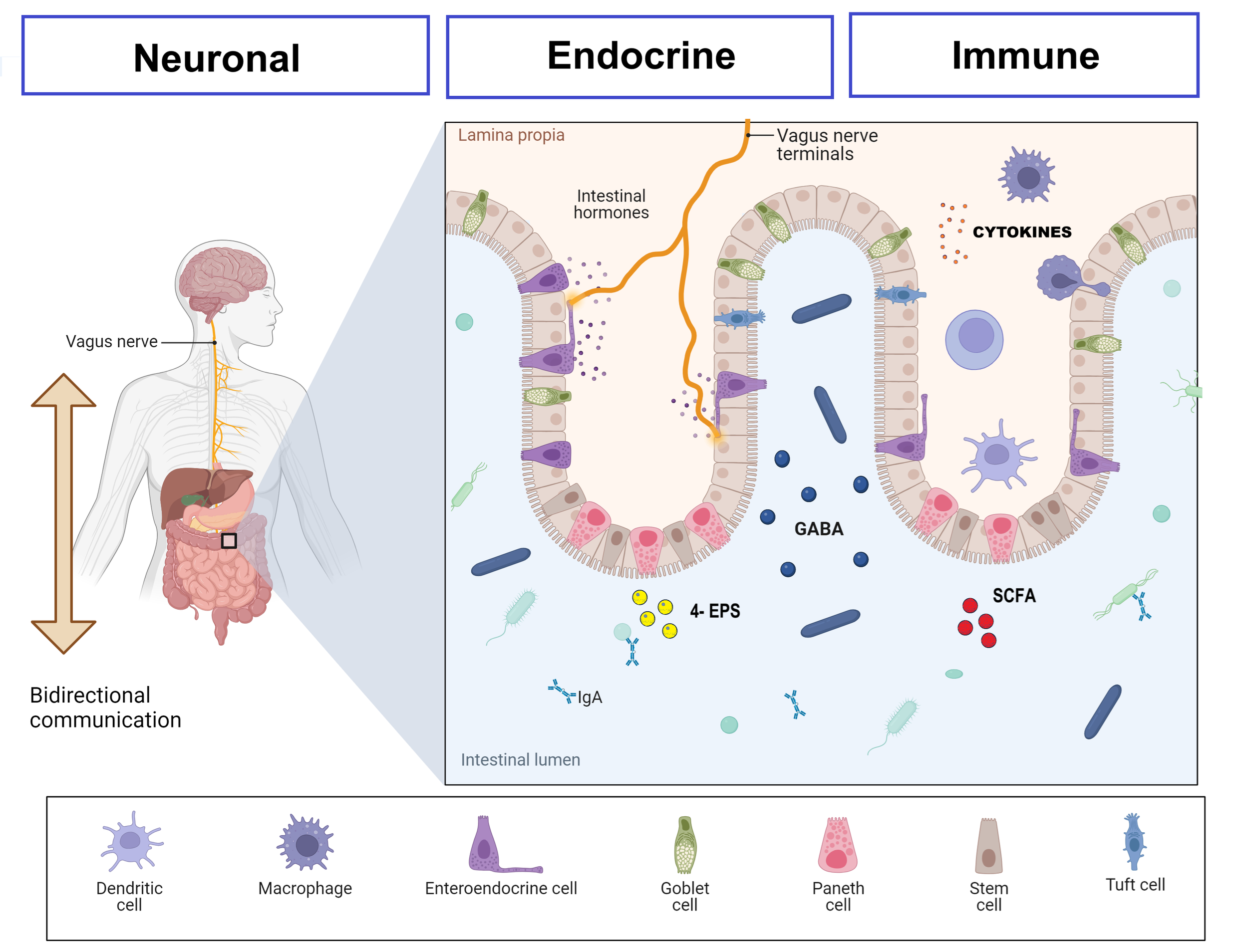
Many ancient cultures viewed the gut as the seat of emotions and intuition. The Greeks and Romans believed that vital emotions and instincts resided in the stomach or intestines rather than the brain. After decades of research, scientists have figured out the strong connection between the gut and the brain, where the gut microbiota plays a key role in this bidirectional communication network recognized as the “microbiota-gut-brain axis”. Today, we know that this communication takes place through neural connections, circulating immune cells, and soluble signaling molecules involving the nervous, immune, and endocrine systems (Figure 1).
Figure 1- Major active communication pathways between the gut microbiome and the brain. GABA: Gamma aminobutyric acid. SCFA: Short-chain fatty acids. 4-EPS: 4-Ethylphenyl sulfate. Created with Biorender.
Groundbreaking studies have evidenced the functionality and importance of this intricate network such as the use of gnotobiotic mice in the context of Parkinson´s disease models (1) and the fecal microbiota transplantation depicting the role of gut microbiota in adult hippocampal neurogenesis in the context of Alzheimer´s disease (2). In this sense, our research group at CERELA (Argentina) has also made some contributions, like unveiling how conditioned media derived from specific lactic acid bacteria strains could improve key molecular events linked to Alzheimer´s disease pathology in vitro (3). These results were further correlated with in vivo studies and presented at the 2023 ISAPP annual meeting in Denver (Figure 2). Recent innovative studies have shown that gut microbiota plays a crucial role in this interaction, influencing neurotransmitter production, inflammatory responses, and even brain plasticity.
The Role of Gut Microbiota Signals in Neurodegenerative Diseases
Mounting evidence suggests that gut microbiota dysbiosis—an imbalance in microbial composition—plays a significant role in neurodegenerative diseases such as Alzheimer’s disease (AD), Parkinson’s disease (PD), and Multiple Sclerosis (MS) through mechanisms mediated by the gut-brain axis (4). Gut microbiota influences neuroinflammation, oxidative stress, protein aggregation, and neurotransmitter production, all of which are key players in neurodegeneration.
Figure 2- Pablo Cataldo presenting at ISAPP annual meeting in Denver (2023). Photo by: Natalia Rios Colombo.
In Alzheimer’s disease, several studies performed with different mice models showed that the development of AD pathologies, including Aβ plaque, hyperphosphorylated tau, synaptic dysfunction, and microglial activation appears to be influenced by the gut microbiome (5). Moreover, a recent report by Grabrucker, Marizzoni (2) evidenced how gut microbiota from AD patients harmed adult hippocampal neurogenesis in mice after fecal microbiota transplantation (FMT), with cognitive and behavioral consequences. In Parkinson’s disease (PD), the gut has emerged as a potential origin site for alpha-synuclein (α-syn) misfolding, a pathological process that leads to the loss of dopaminergic neurons. The “gut-first” hypothesis of PD suggests that certain gut microbes can induce misfolding of α-syn, which then spreads to the central nervous system (6). In Multiple Sclerosis (MS), an autoimmune neurodegenerative disease, gut microbiota is thought to play a role in modulating neuroinflammation and immune responses. In MS patients, the gut microbiota influences immune function via modulation of serotonin production in the gut and through complex interactions with components of the immune system, such as T cells and B cells (7).
Together, these findings suggest that targeting the gut microbiota through dietary interventions, pre-, pro-, postbiotics and FMT may offer promising new therapeutic strategies for neurodegenerative diseases. However, significant challenges remain, including understanding the precise microbial mechanisms involved and developing targeted interventions that can effectively modulate the microbiome without unintended side effects.
Innovative Tools to Study the Gut-Brain Axis: The Role of Organ-on-a-Chip
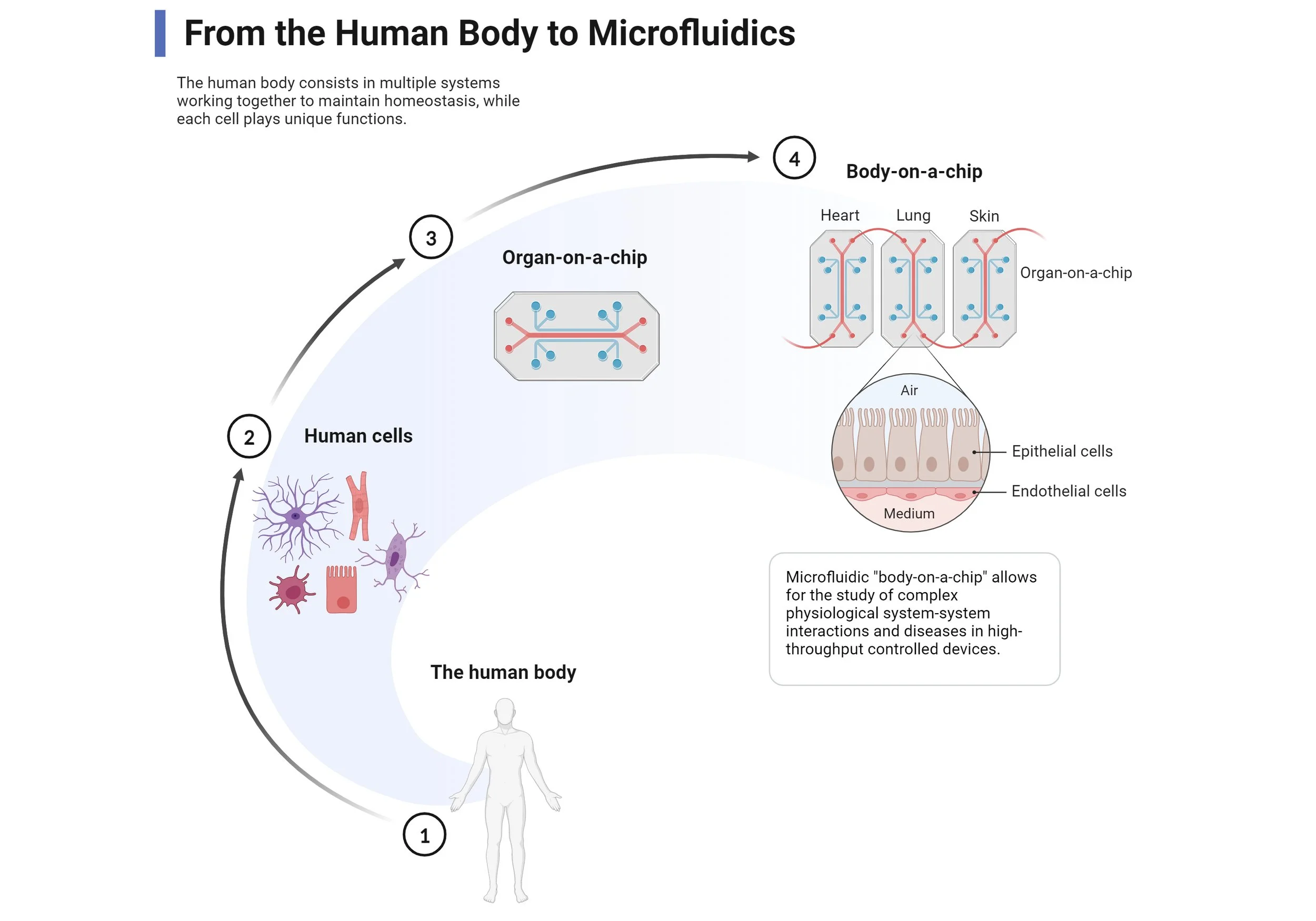
Traditional models such as regular in vitro assays and animal studies have provided crucial insights but have limitations in mimicking human physiology. In this sense, Organ-on-a-chip technology represents a cutting-edge alternative, allowing researchers to recreate gut-brain interactions using microfluidic platforms that simulate the intestinal and neural environments (Figure 3).
Figure 3- Representation of an organ-on-chip developmental process. Created with Biorender.
The MINERVA project first proposed a comprehensive physical model of the microbiota-gut-brain axis consisting of five organ-on-a-chip devices corresponding to the gut microbiota, gut epithelium, the immune system, the blood-brain barrier, and the brain (8). This technology offers greater control, reproducibility, and the potential for personalized medicine, bringing us closer to understanding the gut-brain connection at a mechanistic level (8). Though this technology is still a reductionist approach I think its complexity and ongoing development hold potential to fill the gaps between current in vitro assays and animal models. In this sense, I recommend listening to the ISAPP podcast interview with prof. Kerensa Broersen, where she explains her latest work with a model of the gut-brain axis on a microfluidic chip.
Challenges and Future Directions: Bridging the Gaps
Despite significant progress, key challenges remain in gut-brain axis research:
- The mechanisms of microbiota-host communication are still not fully understood, with many pathways yet to be uncovered.
- Limited clinical studies hinder the translation of preclinical findings into human therapies. Thus, more targeted, large-scale, and well-controlled trials are needed.
- There is a need for better experimental models that accurately reflect the complexity of gut-brain interactions, with improved reproducibility and human relevance. Gut-brain-axis on-chip technologies remain a promising research strategy!
Addressing these challenges will be crucial for developing microbiota-based interventions for neurological and psychiatric disorders.
References:
1. Sampson TR, Debelius JW, Thron T, Janssen S, Shastri GG, Ilhan ZE, et al. Gut microbiota regulate motor deficits and neuroinflammation in a model of Parkinson’s disease. 2016;167(6):1469-80. e12.
2. Grabrucker S, Marizzoni M, Silajdžić E, Lopizzo N, Mombelli E, Nicolas S, et al. Microbiota from Alzheimer’s patients induce deficits in cognition and hippocampal neurogenesis. Brain. 2023;146(12):4916-34.
3. Bulacios GA, Cataldo PG, Naja JR, de Chaves EP, Taranto MP, Minahk CJ, et al. Improvement of Key Molecular Events Linked to Alzheimer’s Disease Pathology Using Postbiotics. 2023;8(50):48042-9.
4. Philip Mani A, Balasubramanian B, Mali LA, Joseph KS, Meyyazhagan A, Pappuswamy M, et al. The Role of the Gut Microbiota in Neurodegenerative Diseases. Microbiology Research [Internet]. 2024; 15(2):[489-507 pp.].
5. Loh JS, Mak WQ, Tan LKS, Ng CX, Chan HH, Yeow SH, et al. Microbiota–gut–brain axis and its therapeutic applications in neurodegenerative diseases. Signal Transduction and Targeted Therapy. 2024;9(1):37.
6. Morais LH, Schreiber HL, Mazmanian SK. The gut microbiota–brain axis in behaviour and brain disorders. Nature Reviews Microbiology. 2021;19(4):241-55.
7. Correale J, Hohlfeld R, Baranzini SE. The role of the gut microbiota in multiple sclerosis. Nature Reviews Neurology. 2022;18(9):544-58.
8. Moradian H, Tristan G, Mathilde B, Xavier R, and Paul S. New methods to unveil host-microbe interaction mechanisms along the microbiota-gut-brain-axis. Gut Microbes. 2024;16(1):2351520.